The Estonian Health Insurance Fund (EHIF) took a big leap towards value-based healthcare as they started a national stroke patient pathway pilot involving 4 out of 6 hospitals in Estonia providing acute stroke care. A visual dashboard was built to display results and enable benchmarking between the hospitals. What information does the dashboard display? How is the information used to improve the stroke patient pathway? What has been successful and what are the lessons learned? We asked EHIF’s Chief Specialist Mariliis Põld and The North Estonia Medical Centre’s Member of the Management Board Terje Peetso and Project Manager Triin Naudi. The North Estonia Medical Centre is one of the four hospitals involved in the pilot.
In this third blog post, we focus on the visual dashboard and how results are utilized to improve the patient pathway. Our first blog post, Better quality of life for stroke patients discusses how this unique national pilot, putting the patient at the center and trying out various incentives to make the pathway better, got started. Further, the project was presented at the ICHOM conference 2020. In the second blog post, Engaging patients in collecting PROMs we discuss starting collecting PROMs and how to engage the patients.
PROM information has been collected for almost a year now. How is the information displayed?
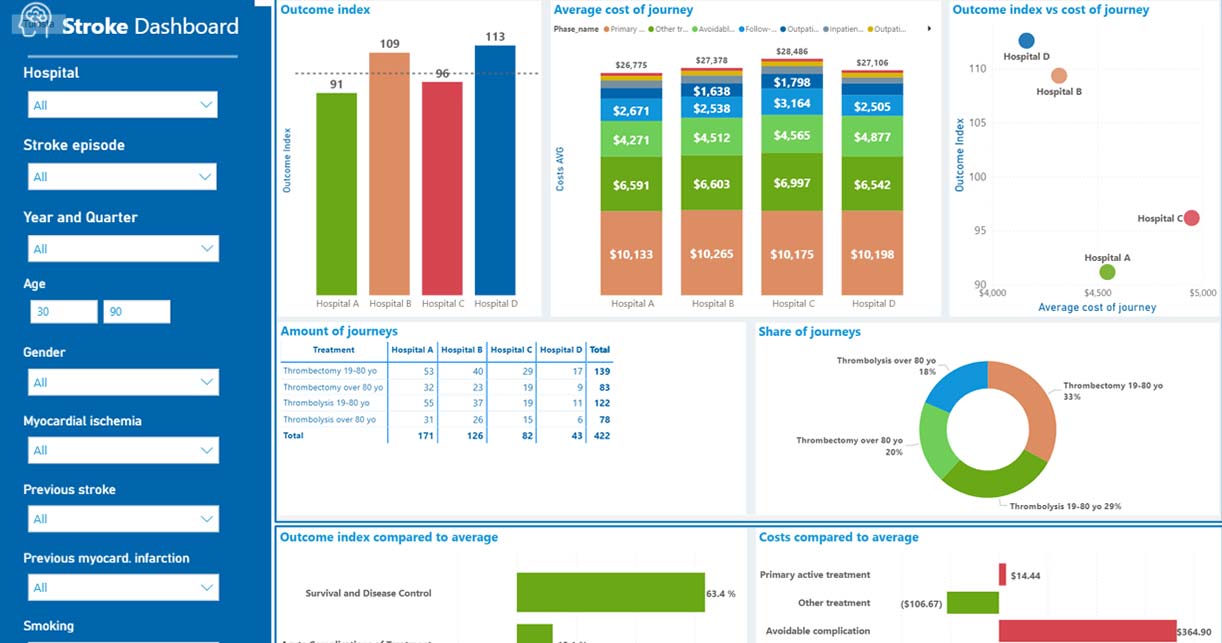
A vital part for utilizing patient reported outcomes (PROM) information to improve the patient pathway is displaying the results. For this purpose, Nordic Healthcare Group (NHG) built a visual dashboard, combining the data from the hospitals and calculating the results, including outcomes and cost data for all four hospitals involved. The dashboard, including information on all involved hospitals, is accessible by both EHIF and the hospitals.
The dashboard presents both cost and outcomes data parallelly which allows professionals to compare outcomes and the costs between the separate hospitals, patient groups and care paths. The dashboard provides an opportunity to deep dive into specific dimensions of the stroke standard set and costs by care pathway step. In the future, standardising the outcomes in regard to the patients’ baseline situation enables comparable indicators, such as the patients’ ability to function, the success of returning to employment, and the flow of the care process.
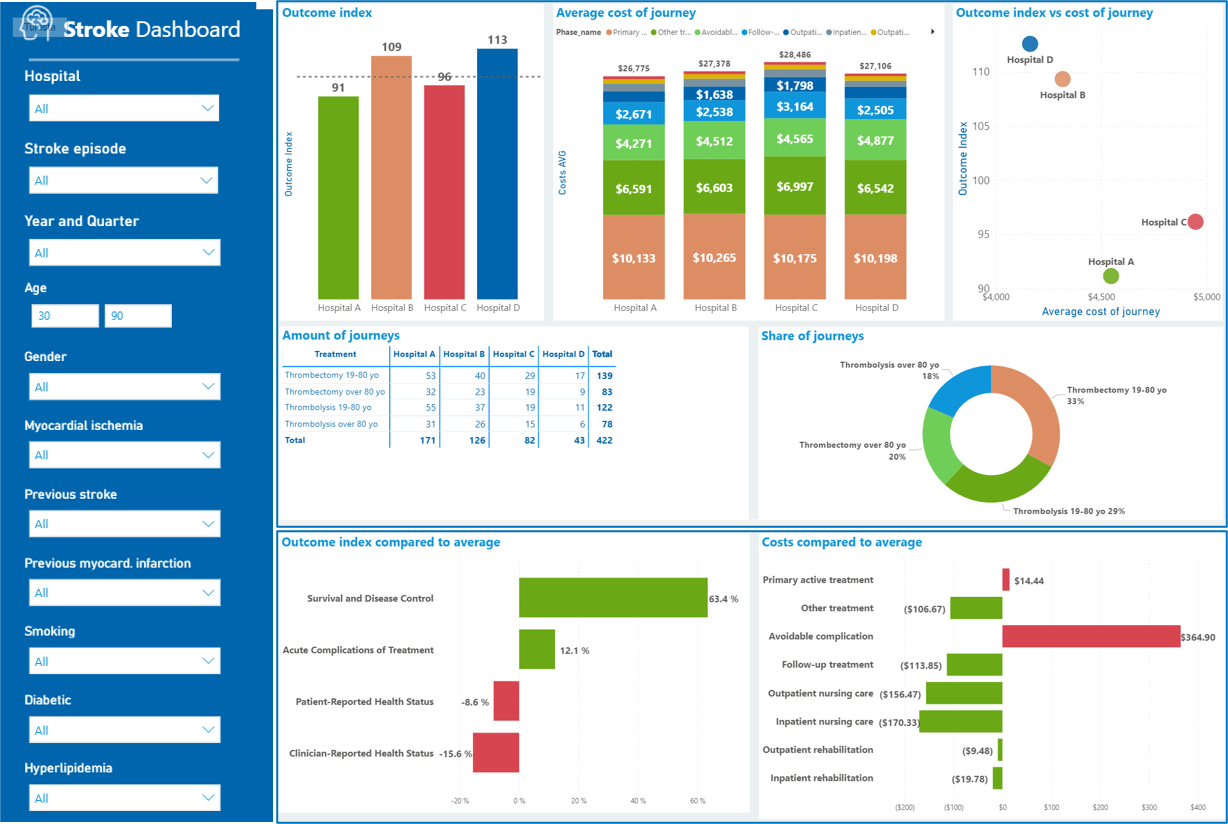
Dashboard view: anonymised and translated version including overall view of both outcomes and costs, deviation analysis showing where a selected hospital is scoring well and where it can improve, outcome index summarising different dimensions of the ICHOM standard set, possibility to case mix adjust the results, and other filtering possibilities.
How did you at EHIF get started in building the dashboard? What has needs to be taken into account?
When starting to draft the dashboard, we at EHIF had the idea of a very visual place with the possibility to manage costs and expected costs compared with patient outcome data. Our other objective was to create a helpful tool to assess the success of the project. We visioned a tool that helps making conclusions on best practices and finding challenges to be tackled. Important factors were visuality, interactivity, and the possibility to filter different groups and variables as well as to compare different hospitals and patient groups.
When reviewing our idea for the dashboard, a document from 1-1,5 year ago, compared to the real situation of today, we are pleased to see that most of what we wanted and dared to dream about is actually there. We are very satisfied with how the dashboard turned out: you can see the cost data and outcome data divided into three categories: process related indicators, patient reported indicators and indicators describing the administrative side.
How do the hospitals use the dashboard and information displayed on it? Have the results been used at the North Estonian Medical Centre to improve the stroke patient pathway?
First of all, at this point, we must understand that the dashboard was only recently launched and, hence, we are only beginning to see all the benefits.
The dashboard is not a clinical evaluation tool but rather we use it to see what impact different interventions we are piloting have, for example 3 months after stroke on the patient’s quality of life and mental and physical health. Thus, with help of the dashboard, we measure if our “pilots inside the pilot” are successful.
PROMs include metrics on what influences the patient’s quality of life and, therefore, we can now create better processes supporting the patient needs. How could we get this closer to the medical understanding? This would require a user friendly, automated dashboard such as an open electronic health record: what has been done and what has come out of it? The stroke patient pathway pilot is run from a process-oriented perspective, but we at hospital level would like to focus in the future more on how to choose the best treatment option for the patient based on the information displayed. Additional data points to the standard set would be helpful to see more clearly the correlation between interventions and results.
What has been successful with the dashboard?
From the hospitals point of view, the data sets become an essential part of the quality indicators. The data is a good indicator to get an overall understanding for development purposes. It is best used, not to control, but improve practices. In the ICHOM standard set, one benefit is that the patients give their input not only during visits at the hospital but also in between. This is a good source of understanding to what could be done differently - a modern approach to quality indicators taking into account the doctors’ and the patient’s view.
It is very interesting to get insight on PROMs and comparing it to cost data and, further, comparing with the other hospitals’ results, for example, patient reported physical health, or patient reported mental health. For patient reported outcomes, we can see the change in time and compare between hospitals. Certainly, interesting discussions will follow between the hospitals when the dashboard is fully live. The hospitals are already thinking about difference is the outcomes data and trying to find factors behind the differences.
With the help of the dashboard, we at the hospitals already see potential to improve the patient pathway by finding new effective intervention methods, for example extending rehabilitation could be a possibility. In this regard, the specialist associations should take ownership of the data and agree on the next steps.
What are the lessons learned?
Lesson 1: Doctors and patients are interested in different information
A study in the British Medical Journal in 2017 by Marc Harrison showed that professionals and patients are looking for different outcomes. In contrary to the doctors, patients are not interested in mortality or complications, but rather in the process influencing their everyday life, such as how often to take the medicine and what the patient rooms look like in the hospital. This could also be better represented in the ICHOM standard sets: What are we really measuring? How do we take into account patient-reported outcomes measures and the doctors’ interests?
Tip for others: When starting to measure PROMs be mindful of what you are measuring. Be aware that patients and clinicians are interested in different kind of information. What purpose should the information serve?
Lesson 2: The implementation can get time consuming, a platform for collecting PROMs is important
From the hospitals’ perspective, the implementation process can get quite time consuming and require additional resources for example to collect the data. To avoid double data entering, the data should be linked to the electronic health record system of the hospital. Further, the dashboard should then display a view which can be used to support everyday work. Further, to avoid additional manual work, patients should be able to enter PROM information digitally themselves. We would also like to point out the importance of using a platform for collecting PROMs when starting an implementation in other therapeutic areas to support the learning process.
From EHIF’s perspective, the dashboard has become more packed than intended originally. Therefore, the dashboard takes some time to get used to in the beginning but on the other hand important features cannot be left out. Unfortunately, not everything can be foreseen in the planning phase but we are thankful to our development partner NHG to be able to incorporate the needed add-ons.
Tip for others: The technical side can become an issue, if you don’t put effort into making the platform user-friendly. Plan carefully ahead how the information can be linked as easily as possible into existing systems and everyday work. Still, there will be things to add afterwards, hence, be prepared to have flexibility in the development of the dashboard.
Lesson 3: Consider the best patient group to start with when measuring PROMs
When planning for an implementation, be sure to consider the patient group carefully. From the hospitals point of view, stroke is a very complex condition as a first diagnosis to be piloted. Merely, the age of the patients can make data collection difficult. For example, stroke patients may have speaking difficulties, memory problems, they do not hear well on the phone or are not digitally capable. Practical issues in PROM collection need to be considered as well, e.g., stroke patients might get tired after already a few questions. Further, stroke is very individual and the health condition of patients after stroke varies widely.
On the other hand, from EHIF’s perspective, a new project is being prepared for hip and knee replacements. After the stroke patient pathway, this seems easy. So, starting out with a complex condition makes future projects seem easier.
Tip for others: Be aware of the pros and cons when choosing the patient group and condition for your trial. Maybe it would be wise to start out the first pilot with a patient group similar to each other where the pathway is not that complex. Consider also the digital capabilities and possibilities to collect PROMs from the patient group.
Want to hear how this story continues?
In our next blog post on this ICHOM & Nordic Healthcare Group blog, we will discuss further benchmarking of PROM results. We will also hear how the bundled payment model has been working. Follow up on the blog.
Written by Milja Saarimaa, Communications and Marketing Manager at Nordic Healthcare Group (NHG) based on the interview of EHIF’s Chief Specialist Mariliis Põld and The North Estonia Medical Centre’s Member of the Board Terje Peetso and Project Manager Triin Naudi. NHG is ICHOM’s certified implementation partner in the Nordic region and proud to assist EHIF in the project.
Estonian Health Insurance Fund is a single payor in Estonian health care system covering the costs of health services required by the person in case of illness. Our mission is to cover the costs of 1,2 million people for their health services, to help prevent and cure disease, finance the purchasing of medicinal products and medicinal technical aids, and provide the benefits for temporary incapacity for work and other benefits.
Nordic Healthcare Group (NHG) is a Finnish based company founded in 2004, expanding in the Nordics and internationally. NHG is specialising in supporting quality services for social and healthcare. Our clients include hospital districts, municipalities, private service providers, pharmaceutical companies, private equity investors and healthcare technology companies. We employ more than 140 experienced professionals. In 2019, NHG became ICHOM’s (International Consortium for Health Outcomes Measurement) certified implementation partner in the Nordic region.