Better quality of life for stroke patients
A unique national stroke patient pathway pilot puts patient at the centre and tries out various incentives to make the pathway better.
The Estonian Health Insurance Fund (EHIF) took a big leap towards value-based healthcare as they started a national stroke patient pathway pilot involving 4 out of 6 hospitals in Estonia providing acute stroke care. How did this project get started? What has been successful so far? And most important, what are the lessons learned? We asked EHIF’s Head of Specialist Care Department Tiina Sats, Innovation Lead Kitty Kubo and Project Manager Rõõt Palmiste.
“The goal of the Stroke Patient Pathway Pilot is to improve patients’ quality of life through developing more integrated care pathway from the patient’s view. The Pilot contains of three major parts – various development projects that four hospitals are leading, for the first time we are starting to measure patient reported outcomes, and testing a new, bundled payment model for the whole stroke care pathway.” – commented Maivi Parv, Member of Management Board, EHIF in a press release on 21th August.
How did you get the idea for this pilot? Why was ischemic stroke chosen?
In 2018, the Association of Neurologists came forward to the Ministry of Social Affairs and the Estonian Health Insurance Fund (EHIF) with problems in stroke care. Two main issues were raised by the specialists: Firstly, the lack of agreement on the transport of acute stroke patients, i.e. that ambulances didn’t transport patients to the right hospitals with stroke units and centres, but instead also to rural hospitals with no stroke units. Secondly, the rehabilitation and other follow-up care of stroke patients was insufficient.
Ischemic stroke is a disease with big impact in Estonia – about 3.200 people suffer from it each year. The mortality of patients within one month after the stroke is approximately 20%, while 45% of the stroke patients who survive will continue their lives with a functional disability of some degree. Due to high disease burden and its fragmented and complicated care pathway, we at EHIF chose ischemic stroke for the first patient pathway pilot project. The aim was to gain deeper understanding to the patients’ side of the story instead of only hearing about the problems from the care providers perspective.
Since the initial proposal to develop the stroke patients’ care came from the specialists, we captured the momentum to start a big national pilot. We realised that the opportunity to act was now as the stakeholders were already onboard and committed to the goal of creating better quality of life for the stroke patient.
How did the pilot get started?
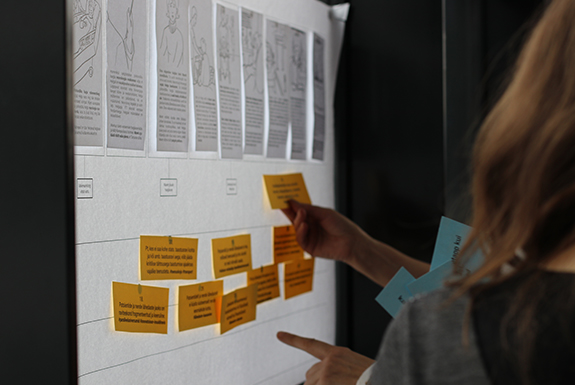
First, we needed to gain clear understanding of the situation and what the better pathway might be. Our goal from day one was to put patient at the centre. Through the discussion we tried to get an understanding what was problematic from the patients’ view. We engaged service designers and interviewed patients and specialists.
In 2019, we invited all stakeholders within stroke care to a service design workshop. We really wanted to dive deep into what the actual problems were and what we could do to solve them? What should we achieve during the next 5 years? What will be better in 5 years?
At first, we discovered that one main issue was the lack of care integration. The patient pathway was fragmented. The patients were not informed on the nature of stroke and not involved in the decision making of next steps in their treatment. The lack of coordination and communication lead to the situation they didn’t get the services they needed (e.g. mental health issues, rehabilitation). The responsibility to arrange services needed lay too heavily on the patient or his closed ones.
Another issue we discovered, was that we measure process in hospitals, but we don’t have the fact and figures of patient quality of life to support improvement. In the beginning, we asked in the workshops, what will get better? Everyone agreed, that this goal is better quality of life for the patient. But if we do not measure outcomes, how do we know if this result has been achieved?
How did you proceed to get the pilot project going on?
As we discovered through the discussions and workshops with stakeholders, our main problem was not the quality of acute care, which was recognised to be good, but the integration of the patient pathway. After identifying the main challenges, we started designing the pilot project. In the workshops, we discovered, that the innovation itself should take place near the patient. This meant, that instead of a central national level change, we needed to make the change happen at hospital level. To support the change, care providers needed to be equipped with the necessary tools and resources. Thus, we decided on three pillars for a successful pilot project:
1. The development projects at the hospitals are the most important part of the pilot, since the change happens here. The development projects are carried out by the care providers but they get extra funding from the EHIF’s innovation fund.
2. Collecting outcomes is vital to understand the patients’ wellbeing and to improve their health outcomes. Also, to be able to follow if the change happens and if our goals are achieved.
3. Changing the payment into a bundled payment model, where the payment should also support coordination and cooperation.
All 6 hospitals providing acute stroke care in Estonia applied, and 4 of them were chosen for piloting. IT systems supporting the implementation is a vital success factor in the project.
Of course, the issue on, how outcomes should be measured, was also discussed to have a joint understanding. Together with the neurologists and all stakeholders, we decided to choose ICHOM’s stroke standard set, not only because of the PROMs but essentially also because of ICHOM’s case mix data.
Implementation of the pilot was planned as phased. At the end of 2019, the development projects got started in the hospitals. As of 1st July 2020, hospitals started with the outcomes’ measurement and new bundled payment model. We are very excited to get the first half years result soon.
What was successful in getting the pilot running at first?
It was a very good idea to bring together all stakeholders from the beginning to discuss issues from the patient’s perspective. We noticed that the people involved in the patients’ pathway do not meet usually, for example neurologists do not know the other specialists on the pathway. By creating a network around the patient, they were able to see each other’s point of view.
Another success factor was to create a shared vision at the start: better quality of life for stroke patients. In order to make the change happen, a shared understanding of the future was needed. Everyone agreed on a more patient-centred care pathway with continuity. We also discussed from the beginning, that we need to measure outcomes to know, if we have achieved our goal.
Using the momentum, was probably the key to get the change started. The initial proposal to develop the stroke patients’ care came from the specialists and we captured the opportunity to start a big national pilot, at the point when all stakeholders were onboard and excited.
We learned from other countries’ experience that to enable change and make informed decisions, IT-solution to support PROMs collection, benchmarking, as well as management of bundled payment is crucial. As we did not have a suitable solution, we planned to procure an IT-system from the very beginning.
What were the lessons learned?
Lesson 1: Things take more time and resources than expected. For example, it took a lot of time to agree upon the framework. After agreeing on the ICHOM stroke standard set, we did not understand, how much work we still had ahead of us before the implementation could start. A lot of questions needed to be answered: How do we understand the ICHOM standard set? How should the process in the hospitals change, so that we can measure outcomes? How should we use data? We started these discussions too last minute, so the pressure was high to agree on many details fast. Also, things like getting licenses and translation of the questionnaires took time. Providers did not see it takes so much resources, not only for the development work, but also for collecting and measuring outcomes and switching to new payment model.
Tip for others: Take into account, that there is a lot of work in the details. Ensure to start discussions on the details early. Schedule enough time to make sure to have the opportunity to involve all parties in the discussions. Ensure that the care providers involved have an understanding of the resources needed.
Lesson 2: Be clear to create an understanding of the terminology and communicate actively when starting something new. Starting a ground-breaking national pilot project involves many new things, so communication and clarification are key. Value-based healthcare or outcomes-based healthcare were not that familiar in Estonia. This was also the first time in Estonia to measure PROMs and test bundled payment. It takes time, efforts and a lot of explaining and communicating. Also, there were suspicious attitudes towards EHIF’s role, since in Estonia we were generally seen only as a payer of services, not as an innovator and partner. Thus, to avoid misunderstanding, there cannot be too much communication at the beginning.
Tip for others: Are you doing something new and ground-breaking? Remember that value-based healthcare is not that familiar to everyone. Communicate actively and explain terminology to create a shared understanding and commitment.
Lesson 3: Paying for outcomes is not only seen as a positive thing. In the beginning, everyone agreed that outcomes are important to be collected. Later on, providers got back to the question: Why are we doing this? Suspicions can arise, if there can be money lost. We understood from the start that financing based on outcomes is not possible yet, and we need first to learn to measure outcomes before we can link outcomes with payment. We needed to move step by step. Therefore, we started with a bundled payment model without outcomes adjustments.
Tip for others: Paying for outcomes sounds mainly good, but this is a very new approach in healthcare. Be prepared for a lot of questions and even suspicious attitude among for example care providers. Also, the downside needs to be discussed, and transparency, communications and moving step by step are vital factors to a successful change.
Want to hear more about this story?
Join our case presentation “Measuring Outcomes and Stroke Patient Pathway Pilot in Estonia” at the ICHOM conference on Day 3, November 18th at 11:20 CDT.
How will the story continue? To share results of the implementation, the pilot project will be followed-up in another blog post on the ICHOM blog. Stay tuned!
Written by Milja Saarimaa, Communications and Marketing Manager at Nordic Healthcare Group (NHG) based on the interview of EHIF’s Head of Specialist Care Department Tiina Sats, Innovation Lead Kitty Kubo and Project Manager Rõõt Palmiste. NHG is ICHOM’s certified implementation partner in the Nordic region and proud to assist EHIF in the project.
Estonian Health Insurance Fund is a single payor in Estonian health care system covering the costs of health services required by the person in case of illness. Our mission is to cover the costs of 1,2 million people for their health services, to help prevent and cure disease, finance the purchasing of medicinal products and medicinal technical aids, and provide the benefits for temporary incapacity for work and other benefits.
Nordic Healthcare Group (NHG) is a Finnish based company founded in 2004, expanding in the Nordics and internationally. NHG is specialising in supporting quality services for social and healthcare. Our clients include hospital districts, municipalities, private service providers, pharmaceutical companies, private equity investors and healthcare technology companies. We employ more than 140 experienced professionals. In 2019, NHG became ICHOM’s (International Consortium for Health Outcomes Measurement) certified implementation partner in the Nordic region.